Melanoma is a type of skin cancer caused by damage to the DNA of melanocyte cells, which are found in the outer layer of your skin. Melanoma occurs when damaged melanocytes begin to reproduce uncontrollably, forming malignant tumors.
What is Melanoma Skin Cancer?
Jump to section

Melanoma can be cured if it is diagnosed and treated in its earliest stages, before the disease has spread. If melanoma is not addressed quickly, however, it may spread to other areas of the body, including vital organ systems.
When melanoma spreads (a condition called invasive melanoma) it may become difficult or impossible to cure. In these cases, melanoma can be fatal.
What are Melanocytes?
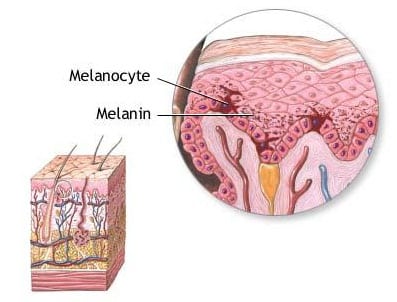
Your skin is made up of several different types of cells, each serving a specific function.
One type of skin cell, called a melanocyte, is responsible for producing melanin, which is the pigment that creates your skin, eye, and hair color. This process is called melanogenesis. Melanocytes are also responsible for the formation of moles on your skin.
Melanocytes are found in the deepest part of the top layer of skin, called the basal layer. They account for about 5 to 10% of the cells in the basal layer.
Signs and Symptoms of Melanoma
The earliest signs of skin cancer involve a change in your skin. This may mean that a new lump or sore has formed, that a new mole has popped up, or that an existing mole has begun to grow or change in shape.
In general, any unusual moles, sores, lumps, blemishes, markings, or changes in the way an area of the skin looks or feels may be a sign that you have melanoma, or a warning that it might occur.
Melanoma is a curable disease when caught early. While not all melanomas show symptoms before spreading, the vast majority of cases begin with an abnormal mole or growth on your skin. If detected during this stage, the cure rate is very high.
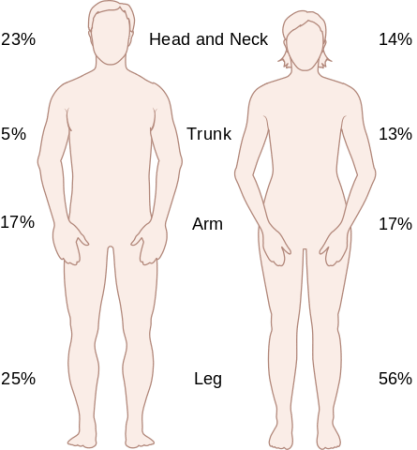
Where Melanoma Forms
Melanoma typically forms on areas of your skin that are frequently exposed to the sun. Particularly vulnerable body parts include your back, legs, arms, and face.
However, melanoma can occur anywhere on your body, including the palms, soles of the feet, and underneath fingernails.
Rarely, melanoma can form in parts of the body other than the skin, such as your mouth, eyes, or intestines.
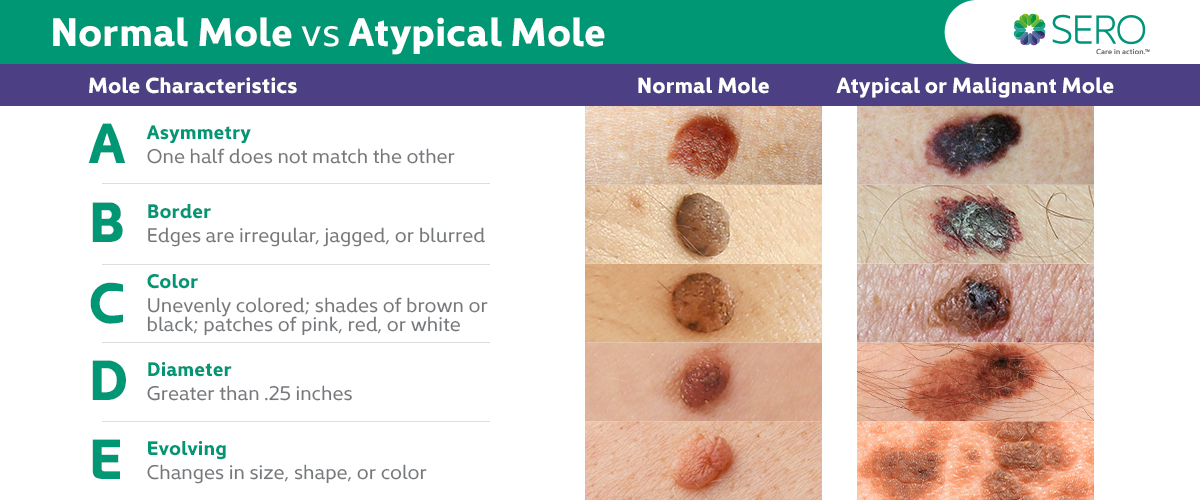
Monitor Your Moles
A melanoma lesion frequently looks like a mole in its earliest stages. Melanomas often appear as black or brown splotches, but may also be pink, white, blue, or purple. While melanoma often looks like a mole, it may also form as normal-looking skin that is sore, sensitive, or itchy.
Moles are a normal part of the body for many people. Most people have between 10 and 50 on their body. Since melanomas often form from existing moles, it’s important to check your skin every few months and to know the signs of melanoma should they appear.
Rarely, melanoma can form in parts of the body other than the skin, such as your mouth, eyes, or intestines.
Melanoma lesions may form suddenly, or may evolve from existing moles. While melanoma can take on many different forms, the general warning sign is a changing or atypical mole.
Consult a doctor if you notice changes in your skin. These may include:
- The sudden appearance of new moles or growths
- Moles that change in size over time (exceeding 1/4 inch)
- Asymetrical moles
- Moles with uneven borders
- Moles that change in color
- Moles that begin to itch, bleed, or become sore.
Diagnosis of Melanoma
By performing frequent self-exams, as well as going regularly to visit the dermatologist, you can protect yourself from the dangers of melanoma.
There are two steps in the process of identifying melanoma:
- Skin exam. During a skin exam, a dermatologist or nurse looks over your skin to identify any unusual marks, lumps, rough patches, moles, freckles, birthmarks, or any pigmented area with an unusual color, size, shape, or texture.
- Biopsy. If an area of your skin is identified as abnormal, and your dermatologist wants to do further analysis, a biopsy may be performed. A biopsy is a minor medical procedure in which an abnormal area of skin is removed with a scalpel and examined under a microscope by a pathologist.
Causes and Risk Factors
Scientists believe that melanoma is primarily caused by two environmental factors: 1) Long-term exposure to UV rays and 2) incidences of brief, intense exposure resulting in severe, blistering sunburns. Both sunlight and UV rays from tanning beds may cause skin damage leading to melanoma. However, as with all cancers, melanoma is likely the result of both environmental and genetic factors.
The following characteristics may put you at greater risk of developing melanoma:
- History of severe, blistering sunburn
- Fair skin (People with less melanin in their skin, those with light-colored eyes and blonde or red hair, and those with freckles, have less built-in protection from UV radiation and are at greater risk of developing melanoma.)
- Frequent sunburns in early childhood
- Family history of skin cancer, especially melanoma
- Having a large number of moles (more than 50) or having atypical moles
- Weakened immune system, caused by medical conditions such as HIV/AIDS, or medical treatments such as chemotherapy
Invasive melanoma is projected to be the fifth most common cancer for men (46,870 cases) and the seventh most common cancer for women (29,510 cases) in 2016.
Melanoma Treatment
Great strides have been made in recent months in the treatment of melanoma, particularly in cases where the disease is in advanced stages and tumors have spread to vital organ systems. Many new drugs have been developed that specifically target and destroy melanoma cells while leaving normal cells unharmed.
In addition to these advancements, there are five standard techniques used to treat melanoma.
Surgery
Removing tumors with surgery is the primary treatment option for melanoma. Depending on the size and location of the tumor and the stage of the disease, the type of surgery may range from minor to very complex.
During treatment, a surgeon will use a local incision to cut out the tumor. They will also remove a thin margin of normal tissue around it, to ensure that all cancer cells have been removed.
Mohs surgery is a common surgical technique for early stage melanoma. During treatment, your doctor (usually a dermatologist), surgically removes one very thin layer of skin at a time at the site of the cancer, checking each layer under a microscope as they go to detect the presence of cancer cells. When they reach a layer with no cancer cells, the surgery is over.
Radiation therapy
Radiation therapy refers to the use of targeted, high-energy radiation to destroy cancer cells while minimizing damage to healthy cells. Melanoma is treated with External Beam Radiation, in which a beam of radiation is directed through your skin to the tumor and the immediate surrounding area in order to destroy the main tumor and any nearby cancer cells. To minimize side effects, the treatments are typically given every day for a number of weeks.
The radiation beam comes from a machine located outside of your body that does not touch your skin or the tumor. Receiving external beam radiation is similar to having an X-ray taken. It is a painless, bloodless procedure.
Chemotherapy
Chemotherapy refers to a type of cancer treatment in which you are given drugs that are designed to kill cancer cells. One or more drugs may be given at a time, either intravenously or orally.
Chemotherapy works by targeting cells within your body that divide rapidly, which is one of the main characteristics of cancer cells. Some normal cells also divide rapidly, such as cells in hair follicles and the digestive tract. These cells are also damaged by chemotherapy, which accounts for many of the side effects you may experience when undergoing treatment.
The radiation beam comes from a machine located outside of your body that does not touch your skin or the tumor. Receiving external beam radiation is similar to having an X-ray taken. It is a painless, bloodless procedure.
Biologic therapy/Immunotherapy
Biologic therapy, also called immunotherapy, refers to a type of cancer treatment in which drugs are given through intravenous infusion. The drugs are designed to stimulate the body’s immune system to attack and kill cancer cells.
Cancer cells often disrupt signals sent by the immune system to identify harmful cells. Biologic therapies restore or increase the activities of specific immune system components or counteract immunosuppressive signals produced by cancer cells.
The radiation beam comes from a machine located outside of your body that does not touch your skin or the tumor. Receiving external beam radiation is similar to having an X-ray taken. It is a painless, bloodless procedure.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to attack cancer cells in very specific ways. Targeted therapies work by destroying or disrupting certain components or communication pathways within cancer cells. Often, these components do not exist in healthy cells. Targeted therapies succeed by damaging cancer cells, causing them to die or preventing them from reproducing, while leaving normal cells alone.
The radiation beam comes from a machine located outside of your body that does not touch your skin or the tumor. Receiving external beam radiation is similar to having an X-ray taken. It is a painless, bloodless procedure.