Outside of skin cancer, prostate cancer is the most common cancer diagnosis among men, affecting more than 3 million US men every year. Roughly 14% of all American men, or one man in every seven, will develop prostate cancer at some point in their lifetimes. Since only males have prostate glands, only males can develop prostate cancer.
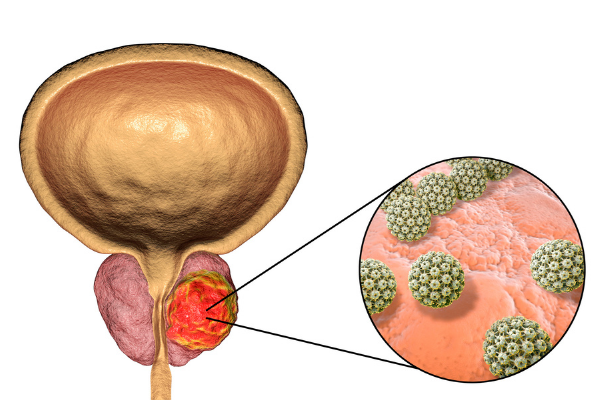
Prostate cancer affects the prostate, a small gland that produces seminal fluid in males. Most prostate cancers do not spread beyond this gland.
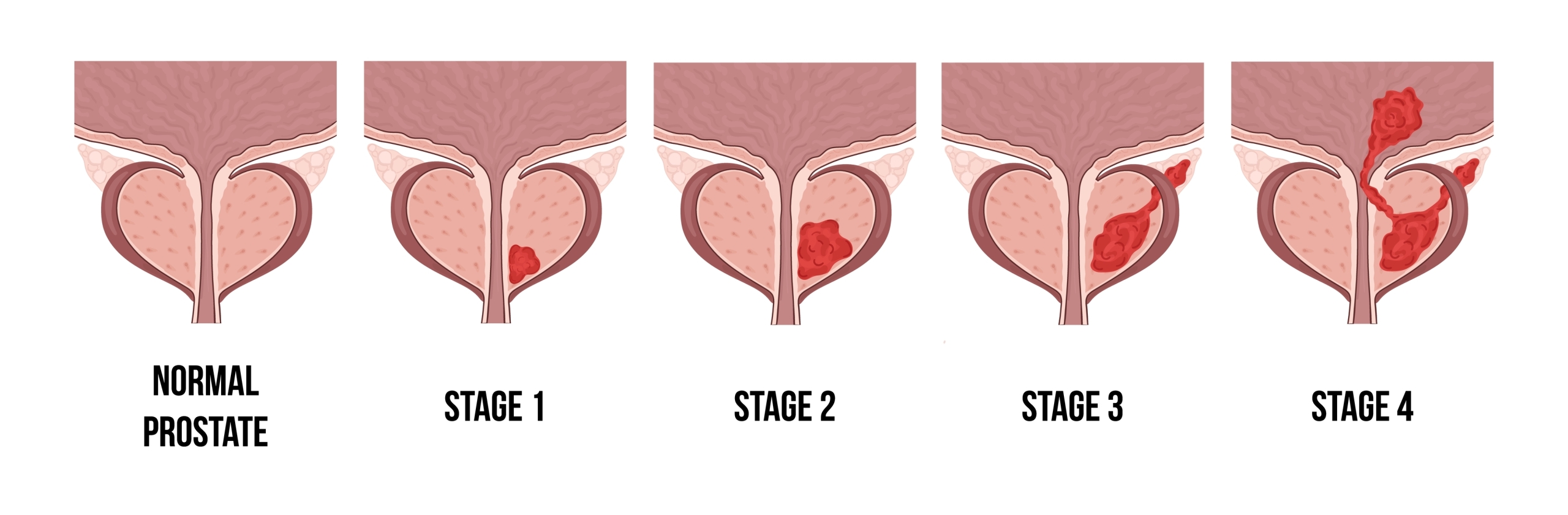
A prostate cancer diagnosis, as with any cancer diagnosis, can seem daunting. However, because many prostate cancers are confined to the prostate gland, they are often treated successfully. Some aggressive prostate cancers do spread quickly, so early detection offers the greatest opportunity for recovery.
If you, a family member, or a friend was recently diagnosed with prostate cancer, it may feel difficult to decide on your next steps. Understanding prostate cancer, its symptoms, and treatment options can help you move forward.