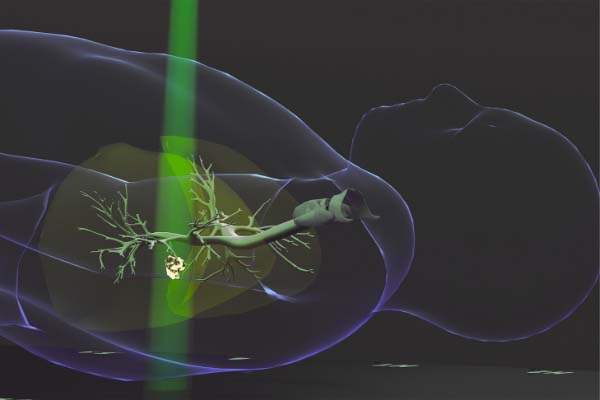
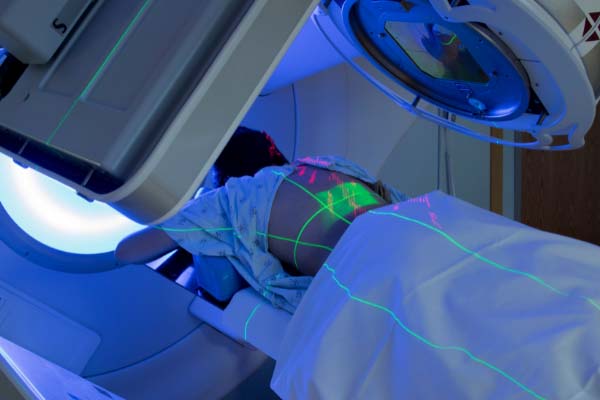
Radiation therapy is one of the most effective and common approaches to cancer treatment, used by leading oncology centers like SERO to target and destroy cancer cells with precision. This painless treatment uses carefully directed high-energy X-ray beams to treat various types of cancer, either as a standalone approach or as part of a comprehensive plan alongside surgery or chemotherapy.
At SERO (Southeast Radiation Oncology Group), our radiation oncologists specialize in using radiation to treat cancer with tailored approaches for each patient’s unique diagnosis. If you or a loved one has recently received a cancer diagnosis in the Charlotte area, understanding how radiation treatment works can help provide peace of mind as you begin your cancer treatment journey.
This comprehensive guide answers the most common questions about radiation therapy for cancer so you can feel informed and confident about your treatment options.