Intraocular melanoma is a rare disease in which cancer forms in melanocytes in the eye. Melanocytes are cells that make melanin (the pigment that gives skin and eyes their color).
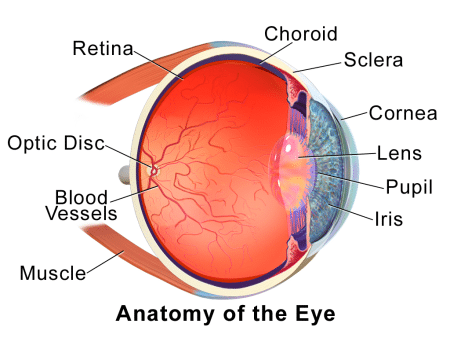
Intraocular melanoma begins in the uvea. The uvea has three parts. The iris is the colored area at the front of the eye. The ciliary body is a ring of muscle tissue that changes the size of the pupil and the shape of the lens. The choroid is a layer of blood vessels that brings oxygen and nutrients to the eye. Most intraocular melanomas begin in the choroid.
There may be no early signs or symptoms of intraocular melanoma. It is sometimes found during an eye exam.
Risk factors for intraocular melanoma include having fair skin that freckles and burns easily, does not tan, or tans poorly and having blue, green, or other light-colored eyes.
- Being older and having fair skin may increase the risk of intraocular melanoma.
- Signs of intraocular melanoma include blurred vision or a dark spot on the iris.
- Tests that examine the eye are used to help detect (find) and diagnose intraocular melanoma.
- A biopsy of the tumor is rarely needed to diagnose intraocular melanoma.
- Certain factors affect prognosis (chance of recovery) and treatment options.